-
PDF
- Split View
-
Views
-
Cite
Cite
Mark McClure, Thomas Jorna, Laura Wilkinson, Joanne Taylor, Elderly patients with chronic kidney disease: do they really need referral to the nephrology clinic?, Clinical Kidney Journal, Volume 10, Issue 5, October 2017, Pages 698–702, https://doi.org/10.1093/ckj/sfx034
Close - Share Icon Share
Abstract
Chronic kidney disease (CKD) is becoming increasingly common, especially in the elderly. In the UK, there has been a marked increase in the awareness and detection of CKD over the last decade. This is largely attributable to the introduction of automated estimated glomerular filtration rate (eGFR) reporting and renal indicators in the primary care Quality and Outcomes Framework (QOF) initiative, both of which were introduced in 2006. These two initiatives have had a significant impact on referral patterns to renal services. Across the UK there has been a sustained increase in patients referred to nephrology clinics. The increased referrals have led to an older patient cohort, for whom specialist nephrology input is of questionable clinical benefit. This study aims to assess the outcomes of such patients referred to nephrology clinics in Dorset.
Retrospective data were collected on all new referrals to the nephrology outpatient clinic at Dorset County Hospital between April 2006 and March 2007. We specifically examined all patients >80 years of age who had CKD Stage 4 or 5. Outcomes of interest included the rate of decline in eGFR, renal-specific management implemented by the clinic, need for renal replacement therapy and death. These outcomes were used to compare the difference between those patients kept under regular follow-up in the nephrology clinic and those discharged back to primary care. Patients were followed up until March 2014.
In all, 124 patients who were ≥80 years of age had CKD Stage 4 (115 patients) or 5 (9 patients). The mean age was 84.4 (range 80–95) years. In all, 66 patients were kept under regular follow-up in the clinic and 58 patients were discharged back to primary care. Patients kept under follow-up tended to have a lower median eGFR at referral (22 mL/min/1.73 m2 versus 26 mL/min/1.73 m2; P = 0.051) and had a significantly more rapid decline in mean eGFR over the next 7 years (1.58 mL/min/1.73 m2/yr versus 0.357 ml/min/1.73 m2/yr; P = 0.023) compared with those discharged back to primary care. More patients were commenced on erythropoietin (12 versus 3; P = 0.03) and more patients were commenced on dialysis (5 versus 0; P = 0.03) in the follow-up group compared with those discharged back to primary care. No patients from either group underwent a kidney biopsy. In those patients followed up, 55 (83%) died, with a median time to death of 2.66 years [interquartile range (IQR) 1.14–4.97]. Of the patients discharged, 45 (78%) died, with a median time to death of 3.57 years (IQR 2.31–5.68).
This study highlights the uncertain clinical benefit gained from referral to the nephrology clinic for the majority of elderly patients and suggests that for many cases their care could be safely and appropriately managed in the primary care setting. With the increasing prevalence of CKD in the elderly and increasing pressure on new patient clinic slots, referral of a select group in which a specific intervention is being considered may be more appropriate.
Introduction
Chronic kidney disease (CKD) is becoming increasingly common, especially in the elderly [1–3]. It is estimated that after the age of 30 years, GFR progressively declines at an average rate of 8 mL/min/1.73 m2/decade [4]. There is considerable debate regarding the significance of this age-related decline in kidney function [5, 6]. As life expectancy continues to improve, there is an increasing prevalence of co-morbidities and risk factors such as hypertension, diabetes and atherosclerosis predisposing to a high burden of CKD in the elderly population. Around half of the population >70 years of age now have an estimated GFR (eGFR) <60 mL/min/1.73 m2 [7].
Many have suggested that this increased recognition of CKD is a positive development and leads to better care in elderly populations [8, 9]. Others have argued that this is a damaging development that has led to many elderly patients being given an unnecessary label without any proven clinical benefit [10]. Elderly patients with advanced CKD often have multiple extra-renal comorbidities. The prospects of rehabilitation in such patients tend to be limited and the prognosis is often very poor. In this group, renal replacement therapy often adds little in additional quantity of life and can pose huge additional burdens for patients and their caregivers.
In the UK, there has been a marked increase in the awareness and detection of CKD over the last decade. This is largely attributable to the introduction of automated reporting of eGFR by pathology laboratories across the UK in 2006 [11, 12]. This coincided with a National Health Service–led pay-for-performance programme and renal indicators in the primary care Quality and Outcomes Framework (QOF), also introduced in 2006 [13]. These two initiatives were intended to promote identification of CKD and have had a significant impact on referral patterns to renal services [14]. Across the UK there has been a sustained increase in patients referred to nephrology clinics. The increased referrals have led to an older patient cohort, for whom specialist nephrology input is of questionable clinical benefit. This study aims to assess the outcomes of such patients referred to the nephrology outpatient clinic in Dorset.
Methods
Retrospective data were collected on all new referrals to outpatient clinic at Dorset County Hospital between April 2006 and March 2007. This is a District General Hospital with a regional renal unit covering a population of ∼950 000 in a rural and high socioeconomic area. The majority of patients are of Caucasian origin. We specifically examined all patients >80 years of age who had CKD Stage 4 or 5, defined as an eGFR <30 mL/min/1.73 m2 using an abbreviated Modification of Diet in Renal Disease (MDRD) formula.
Outcomes of interest in this patient group included the rate of decline in eGFR, renal-specific management implemented from the clinic, need for renal replacement therapy and death. These outcomes were used to compare the difference between those patients kept under regular follow-up in the nephrology clinic and those discharged back to primary care. This decision was based on the overall assessment by a consultant nephrologist.
Patients were followed up until March 2014. All statistical analyses were performed using Prism version 6 software (GraphPad Software, La Jolla, CA, USA) and P-values <0.05 were considered statistically significant.
Results
Referral pattern following introduction of automated eGFR reporting in 2006
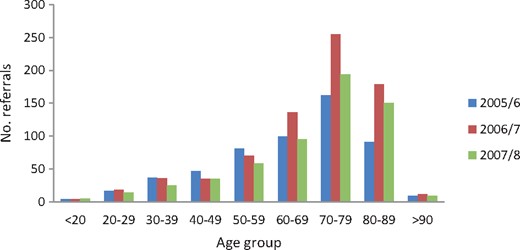
A total of 745 new patients were referred to the nephrology outpatient clinic between April 2006 and March 2007. This was a 36% increase from the previous year. Of these, 136 (18%) were 60–69, 255 (34%) were 70–79 and 179 (24%) were 80–89 years of age. For each age group, this was an increase of 37%, 57% and 97%, respectively, compared with the previous year (Figure 1).
Number of referrals to the nephrology clinic between 2005 and 2008.
Analysis of patients >80 years of age
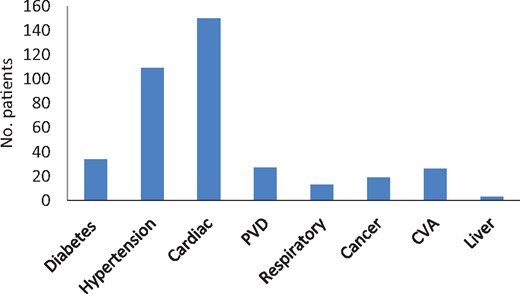
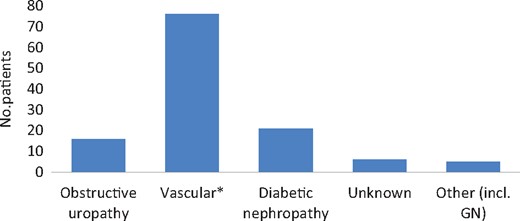
In total, 124 patients who were ≥80 years of age had CKD Stage 4 (115 patients) or 5 (9 patients). The mean age was 84.4 (range 80–95) years and there was no difference in sex distribution (male, n = 65; female, n = 59). The average number of comorbidities was three per patient. These included coronary artery disease (n = 71), congestive cardiac failure (n = 40), hypertension (n = 109), diabetes mellitus (n = 34), peripheral vascular disease (n = 27) and malignancy (n = 19) (Figure 2). The majority of referrals came from primary care (n = 100) and to a lesser extent from medical (n = 22) and surgical specialties (n = 2). Vascular disease (encompassing hypertension and atherosclerotic renal artery disease) was the most common renal diagnosis (n = 76), followed by diabetes (n = 21) and obstructive uropathy (n = 16) (Figure 3).
Comorbidities of patients referred to the nephrology clinic. PVD, peripheral vascular disease; CVA, cerebrovascular accident.
Renal diagnosis as determined by a nephrologist. *Encompasses hypertensive nephropathy and atherosclerotic renal artery disease. GN, glomerulonephritis.
From the >80-years-of-age group, 66 patients were kept under regular follow-up in the clinic and 58 patients were discharged back to primary care. Nine patients were lost to follow-up and three were transferred to different units. Missing data were equally distributed across the follow-up group and the discharged group with no statistical differences. Patients kept under follow-up tended to have a lower median eGFR at referral (22 mL/min/1.73 m2 versus 26 mL/min/1.73 m2; P = 0.05) and had a significantly more rapid decline in mean eGFR over the next 7 years (1.58 mL/min/1.73 m2/year versus 0.357 mL/min/1.73 m2/year; P = 0.02) compared with those discharged back to primary care (Table 1).
Clinical outcomes/interventions for patients >80 years of age who were followed up in the nephrology clinic compared with those discharged back to primary care
| Clinical outcomes/ interventions . | Followed up in the nephrology clinic . | Discharged back to primary care . | P-value . |
|---|---|---|---|
| N | 66 | 58 | 0 |
| Age (years), mean | 85 | 83 | |
| Gender (n), male/female | 30/36 | 32/26 | |
| eGFR at referral (mL/min/1.73 m2) | 22 | 26 | 0.05 |
| Rate of decline of eGFR (mL/min/1.73 m2/year) | 1.58 | 0.357 | 0.02 |
| Comorbidities (n), mean | 3 | 2 | 0 |
| Referred for renal artery angioplasty (n) | 2 | 0 | 0.18 |
| Commenced on cinacalcet (n) | 0 | 0 | 0 |
| Commenced on ESA (n) | 12 | 3 | 0.03 |
| Renal biopsy (n) | 0 | 0 | 0 |
| Commenced on dialysis (n) | 5 | 0 | 0.03 |
| Clinical outcomes/ interventions . | Followed up in the nephrology clinic . | Discharged back to primary care . | P-value . |
|---|---|---|---|
| N | 66 | 58 | 0 |
| Age (years), mean | 85 | 83 | |
| Gender (n), male/female | 30/36 | 32/26 | |
| eGFR at referral (mL/min/1.73 m2) | 22 | 26 | 0.05 |
| Rate of decline of eGFR (mL/min/1.73 m2/year) | 1.58 | 0.357 | 0.02 |
| Comorbidities (n), mean | 3 | 2 | 0 |
| Referred for renal artery angioplasty (n) | 2 | 0 | 0.18 |
| Commenced on cinacalcet (n) | 0 | 0 | 0 |
| Commenced on ESA (n) | 12 | 3 | 0.03 |
| Renal biopsy (n) | 0 | 0 | 0 |
| Commenced on dialysis (n) | 5 | 0 | 0.03 |
ESA, erythropoietin-stimulating agent.
Clinical outcomes/interventions for patients >80 years of age who were followed up in the nephrology clinic compared with those discharged back to primary care
| Clinical outcomes/ interventions . | Followed up in the nephrology clinic . | Discharged back to primary care . | P-value . |
|---|---|---|---|
| N | 66 | 58 | 0 |
| Age (years), mean | 85 | 83 | |
| Gender (n), male/female | 30/36 | 32/26 | |
| eGFR at referral (mL/min/1.73 m2) | 22 | 26 | 0.05 |
| Rate of decline of eGFR (mL/min/1.73 m2/year) | 1.58 | 0.357 | 0.02 |
| Comorbidities (n), mean | 3 | 2 | 0 |
| Referred for renal artery angioplasty (n) | 2 | 0 | 0.18 |
| Commenced on cinacalcet (n) | 0 | 0 | 0 |
| Commenced on ESA (n) | 12 | 3 | 0.03 |
| Renal biopsy (n) | 0 | 0 | 0 |
| Commenced on dialysis (n) | 5 | 0 | 0.03 |
| Clinical outcomes/ interventions . | Followed up in the nephrology clinic . | Discharged back to primary care . | P-value . |
|---|---|---|---|
| N | 66 | 58 | 0 |
| Age (years), mean | 85 | 83 | |
| Gender (n), male/female | 30/36 | 32/26 | |
| eGFR at referral (mL/min/1.73 m2) | 22 | 26 | 0.05 |
| Rate of decline of eGFR (mL/min/1.73 m2/year) | 1.58 | 0.357 | 0.02 |
| Comorbidities (n), mean | 3 | 2 | 0 |
| Referred for renal artery angioplasty (n) | 2 | 0 | 0.18 |
| Commenced on cinacalcet (n) | 0 | 0 | 0 |
| Commenced on ESA (n) | 12 | 3 | 0.03 |
| Renal biopsy (n) | 0 | 0 | 0 |
| Commenced on dialysis (n) | 5 | 0 | 0.03 |
ESA, erythropoietin-stimulating agent.
The average number of comorbidities was higher in the follow-up group (three versus two). More patients were commenced on erythropoietin (12 versus 3; P = 0.03) and more patients were commenced on dialysis (5 versus 0; P = 0.03) in the follow-up group compared with those discharged back to primary care. Two patients received peritoneal dialysis and three received haemodialysis. For these five patients, the duration of dialysis varied from 38 days (haemodialysis patient) to 2 years 8 months (peritoneal dialysis patient) and the maximum lifespan was 5 years 7 months from referral. No patients from either group underwent a kidney biopsy or were prescribed cinacalcet. Two patients from the follow-up group were referred for renal artery angioplasty (2 versus 0; P = 0.18). In those patients followed up, 55 (83%) died, with a median time to death of 2.66 years [interquartile range (IQR) 1.14–4.97]. Of the patients discharged, 45 (78%) died, with a median time to death of 3.57 years (IQR 2.31–5.68).
Discussion
As the UK population continues to age, the incidence and prevalence of CKD in elderly patients is increasing. Nephrologists are increasingly confronted with a population of patients who are elderly and have a large number of comorbidities. Furthermore, the introduction of automated eGFR reporting and renal indicators in the primary care QOF initiative have resulted in a significant and sustained increase in the number of referrals to nephrology clinics across the UK [12–14]. Our unit experienced a similar trend in referral patterns following the introduction of the two initiatives in 2006, with a significant increase in the number of referrals, in particular an increase in referrals of elderly patients.
In our study, the elderly patients kept under regular surveillance in the nephrology clinic tended to have more advanced renal impairment and were more likely to have a rapid decline in kidney function. This suggests that nephrologists were able to correctly identify the patients whom they predicted may require specialist renal input in terms of managing complications of CKD and provision of renal replacement therapy. However, very few patients kept under regular follow-up actually underwent renal-specific intervention and even fewer were started on dialysis. This raises the question of the clinical benefit provided by the nephrology clinic for such elderly patients and suggests that in many cases their care could be safely and appropriately managed in the primary care setting.
It is also worth noting that a significant number of the referrals in this study had obstructive uropathy. This is not surprising given the increased prevalence of prostatic disease in this age group. A renal tract ultrasound prior to nephrology referral could have prompted a more appropriate direct referral to a urologist, which could have expedited management and potentially improved outcomes. It would also have resulted in one less clinic visit and less inconvenience for the patient.
We acknowledge the importance of the early detection of CKD. Controlled clinical trials show that the treatment of early stages of CKD slows down the rate of progression of kidney damage and has beneficial effects on complications [15, 16]. Furthermore, CKD has been shown to be an independent risk factor for cardiovascular events and all-cause mortality, suggesting that early detection of CKD and treatment of its complications seems to be important to improve outcomes in cardiovascular diseases [17–19]. However, it is important to recognize that the vast majority of patients with CKD do not progress to end-stage renal failure (ESRF). This is largely due to the higher competing risk of death among older patients. A study in Norway followed >65 000 patients with CKD Stages 3–5 (eGFR <60 mL/min/1.73 m2) for 8 years. Only 51 progressed to end-stage renal disease and there were 506 cardiovascular deaths. The study highlights that these patients were more likely to die from a cardiovascular event than require dialysis [20]. It is also recognized that the rate of decline in renal function is probably lower in the elderly. A Canadian study followed a cohort of >10 000 elderly patients with CKD and showed that there was either no or minimal progression of CKD over 2 years [21].
For those elderly patients that do reach ESRF, recent reports indicate that dialysis may not provide a clear benefit over conservative care regarding survival and quality of life, especially in those patients with extensive comorbidities. In a number of small comparative studies, dialysis for elderly patients with extensive comorbidities did not confer a significant survival advantage over conservative management [22, 23]. A recent larger study found that elderly patients with extensive comorbidities treated by dialysis had a median survival that was only 5 months longer from entry into CKD Stage 5 than patients who had undergone conservative kidney management [24]. This suggests that an individualized approach is necessary.
For those patients kept under regular follow-up in our study, few received renal-specific treatment and even less were commenced on renal replacement therapy. This highlights the questionable clinical benefit gained from referral to the nephrology clinic for the majority of elderly patients. For patients discharged to primary care, general practitioners (GPs) are advised to follow CKD guidelines. In 2008 the National Institute for Health and Excellence (NICE) published guidelines on the early identification and management of patients with CKD, which was updated in 2014 [25, 26]. Prior to 2008, our local practice was to advise GPs in the discharging letter how often to follow-up patients, what to check, and when to re-refer if appropriate. This advice continued after the formal NICE guidance was introduced. We acknowledge the excellent work performed by GPs throughout the UK. There is published evidence showing that patients with stable early CKD get appropriate monitoring of renal function after discharge from the nephrology clinic to primary care and are also referred back to the renal clinic appropriately [27]. It is, therefore, the responsibility of both the nephrologist and the GP to work in partnership to ensure the provision of good quality care for patients with CKD.
With regard to referral to secondary care, NICE 2014 referral criteria encourage GPs to take into account the individual’s wishes and comorbidities when considering referral [26]. It is important to recognize that the majority of elderly patients with CKD will not ultimately require or desire renal replacement therapy and may be safely managed in the primary care setting. With increasing pressure on new-patient clinic slots, referral of a select group in which a specific intervention is being considered may be more appropriate. Nephrologists also need to play their role to reduce the workload and should be encouraged to discharge such patients back to primary care after initial review in the clinic.
We acknowledge the limitations of this single-centre study. The patient numbers are small and observational data such as these will always generate unavoidable bias and confounding that we were unable to adjust for with our study design. Furthermore, the vast majority of patients in this cohort were Caucasian and our conclusions should therefore be applied with caution to other races.
Conflict of interest statement
None declared.





Comments