Abstract
Background
There are very few studies examining the determinants of frequent attendance in primary care among the oldest old.
Aims
The purpose of this study was to determine the characteristics of frequent attendance among individuals aged 85 years or older.
Methods
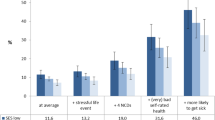
Cross-sectional data stem from the multicenter prospective cohort “Study on needs, health service use, costs and health-related quality of life in a large sample of oldest old primary care patients (85 +)” (AgeQualiDe). This study covers very old primary care patients (n = 861, mean age of 89.0 years ± 2.9; 85–100 years). The number of self-reported GP visits in the preceding 3 months was used to quantify frequent attenders. We defined patients in the top decile as frequent attenders.
Results
Multiple logistic regressions showed that frequent attendance was associated with more chronic diseases (adjusted OR 1.12, 95% CI 1.01–1.23), worse functioning (OR 0.97, 95% CI 0.95–0.99), worries about one’s financial situation (OR 2.20, 95% CI 1.07–4.53) and it was inversely associated with depression (OR 0.26, 95% CI 0.08–0.80).
Discussion
In contrast to studies based on younger samples, different factors were associated with frequent users in our study, showing that it is important to study the determinants of frequent attendance among the oldest old.
Conclusion
In Germany, among the group of the oldest old, frequent attendance was positively associated with worse physical health status (e.g., number of chronic diseases), but negatively with depression. This might indicate that the German health care system is responsive to the physical, but not psychological needs of the oldest old.


Similar content being viewed by others
References
Von Korff M, Ormel J, Katon W et al (1992) Disability and depression among high utilizers of health care: a longitudinal analysis. Arch Gen Psychiatry 49:91–100
van den Bussche H, Kaduszkiewicz H, Schäfer I et al (2016) Overutilization of ambulatory medical care in the elderly German population? An empirical study based on national insurance claims data and a review of foreign studies. BMC Health Serv Res 16:1
Welzel FD, Stein J, Hajek A et al (2017) Frequent attenders in late life in primary care: a systematic review of European studies. BMC Fam Pract 18:104
Hajek A, Bock J-O, König H-H et al (2017) Association of general psychological factors with frequent attendance in primary care: a population-based cross-sectional observational study. BMC Fam Pract 18:48
Cruwys T, Wakefield J, Sani F, Dingle GA, Jetten J (2018) Social isolation predicts frequent attendance in primary care. Ann Behav Med 52:817–829. https://doi.org/10.1093/abm/kax054
Hajek A, Bock J-O, König H-H et al (2017) Which factors affect health care use among older Germans? Results of the German ageing survey. BMC Health Serv Res 17:30
Zok K (2007) Warten auf den Arzttermin. Ergebnisse einer Repräsentativumfrage unter GKV-und PKV-Versicherten WIdO-monitor 4:1–7
Passon A, Lüngen M, Gerber A, Redaelli M, Stock S (2013) Das Krankenversicherungssystem in Deutschland. In: Lauterbach KW, Stock S, Brunner H (eds) Gesundheitsökonomie Lehrbuch für Mediziner und andere Gesundheitsberufe 3. Bern, Huber
Luck T, Rodriguez FS, Wiese B et al (2017) Advance directives and power of attorney for health care in the oldest-old—results of the AgeQualiDe study. BMC Geriatr 17:85. https://doi.org/10.1186/s12877-017-0482-8
Smits FT, Brouwer HJ, Schene AH et al (2016) Is frequent attendance of longer duration related to less transient episodes of care? A retrospective analysis of transient and chronic episodes of care. BMJ Open 6:e012563
Jorgensen JT, Andersen JS, Tjonneland A et al (2016) Determinants of frequent attendance in Danish general practice: a cohort-based cross-sectional study. BMC Fam Pract 17:9. https://doi.org/10.1186/s12875-016-0412-4
Reisberg B, Ferris SH, de Leon MJ et al (1982) The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiat 139:1136–1139. https://doi.org/10.1176/ajp.139.9.1136
Yesavage JA, Sheikh JI (1986) 9/Geriatric Depression Scale (GDS). Clin Gerontol 5:165–173. https://doi.org/10.1300/J018v05n01_09
Gauggel S, Birkner B (1999) Validity and reliability of a German version of the Geriatric Depression Scale (GDS). Zeitschrift fur Klinische Psychologie-Forschung und Praxis 28:18–27
Sheikh JI, Yesavage JA (1986) Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 5(1–2):165–173
Yesavage JA, Brink TL, Rose TL et al (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Mahoney FI, Barthel DW (1965) Functional evaluation: the barthel index. Maryland State Med J 14:61–65
Graf von der Schulenburg J, Claes C, Greiner W et al (1998) The German Version of the Euro-Qol Questionnaire. J Publ Health/Zeitschrift für Gesundheitswissenschaften 6:2–20
Lubben J, Blozik E, Gillmann G et al (2006) Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist 46:503–513
König W, Lüttinger P, Müller W (1988) A comparative analysis of the development and structure of educational systems: methodological foundations and the construction of a comparative educational scale. Universität Mannheim, Institut für Sozialwissenschaften
Van Oostrom SH, Picavet HSJ, De Bruin SR et al (2014) Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam Pract 15:61
Welzel FD, Stein J, Hajek A et al (2017) Frequent attenders in late life in primary care: a systematic review of European studies. BMC Fam Pract 18:14. https://doi.org/10.1186/s12875-017-0700-7
Rennemark M, Holst G, Fagerstrom C et al (2009) Factors related to frequent usage of the primary healthcare services in old age: findings from The Swedish National Study on Aging and Care. Health Soc Care Community 17:301–311. https://doi.org/10.1111/j.1365-2524.2008.00829.x
Vedsted P, Christensen MB (2005) Frequent attenders in general practice care: a literature review with special reference to methodological considerations. Public Health 119:118–137. https://doi.org/10.1016/j.puhe.2004.03.007
Press Y, Tandeter H, Romem P et al (2012) Depressive symptomatology as a risk factor for increased health service utilization among elderly patients in primary care. Arch Gerontol Geriatr 54:127–130. https://doi.org/10.1016/j.archger.2011.02.009
Menchetti M, Cevenini N, De Ronchi D et al (2006) Depression and frequent attendance in elderly primary care patients. Gen Hosp Psychiatry 28:119–124. https://doi.org/10.1016/j.genhosppsych.2005.10.007
Wuthrich VM, Frei J (2015) Barriers to treatment for older adults seeking psychological therapy. Int Psychogeriatr 27:1227–1236
Hand C, McColl MA, Birtwhistle R et al (2014) Social isolation in older adults who are frequent users of primary care services. Canadian Family Physician Medecin de Famille Canadien 60:e322 (e324–329)
Valtorta NK, Moore DC, Barron L et al (2018) Older adults' social relationships and health care utilization: a systematic review. Am J Public Health 108:e1–e10. https://doi.org/10.2105/ajph.2017.304256
Watson D (1988) Intraindividual and interindividual analyses of positive and negative affect: their relation to health complaints, perceived stress, and daily activities. J Pers Soc Psychol 54:1020
Tille F, Gibis B, Balke K et al (2017) Sociodemographic and health-related determinants of health care utilisation and access to primary and specialist care: Results of a nationwide population survey in Germany (2006–2016)]. Zeitschrift fur Evidenz, Fortbildung und Qualitat im Gesundheitswesen 126:52–65. https://doi.org/10.1016/j.zefq.2017.07.012
Bhandari A, Wagner T (2006) Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev 63:217–235
Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J et al (2014) Multimorbidity patterns: a systematic review. J Clin Epidemiol 67:254–266
Fabbri E, Zoli M, Gonzalez-Freire M et al (2015) Aging and multimorbidity: new tasks, priorities, and frontiers for integrated gerontological and clinical research. J Am Med Dir Assoc 16:640–647
Yarnall AJ, Sayer AA, Clegg A et al (2017) New horizons in multimorbidity in older adults. Age Ageing 46:882–888
Acknowledgements
We want to thank both all participating patients and their general practitioners for their good collaboration. Members of the AgeCoDe & AgeQualiDe Study Group: Wolfgang Maier (Principal Investigator), Martin Scherer (Principal Investigator), Steffi G. Riedel-Heller (Principal Investigator), Heinz-Harald Abholz, Christian Brettschneider, Cadja Bachmann, Horst Bickel, Wolfgang Blank, Sandra Eifflaender-Gorfer, Marion Eisele, Annette Ernst, Angela Fuchs, André Hajek, Kathrin Heser, Frank Jessen, Hanna Kaduszkiewicz, Teresa Kaufeler, Mirjam Köhler, Hans-Helmut König, Alexander Koppara, Diana Lubisch, Tobias Luck, Dagmar Lühmann, Melanie Luppa, Tina Mallon, Manfred Mayer, Edelgard Mösch, Michael Pentzek, Jana Prokein, Alfredo Ramirez, Susanne Roehr, Anna Schumacher, Janine Stein, Susanne Steinmann, Franziska Tebarth, Hendrik van den Bussche (Principal Investigator 2002–2011), Carolin van der Leeden, Michael Wagner, Klaus Weckbecker, Dagmar Weeg, Jochen Werle, Siegfried Weyerer, Birgitt Wiese, Steffen Wolfsgruber, Thomas Zimmermann.
Funding
This publication is part of the German Research Network on Dementia (KND), the German Research Network on Degenerative Dementia (KNDD; German Study on Ageing, Cognition and Dementia in Primary Care Patients; AgeCoDe), and the Health Service Research Initiative (Study on Needs, health service use, costs and health-related quality of life in a large sample of oldest-old primary care patients (85 + ; AgeQualiDe)) and was funded by the German Federal Ministry of Education and Research (Grants KND: 01GI0102, 01GI0420, 01GI0422, 01GI0423, 01GI0429, 01GI0431, 01GI0433, 01GI0434; Grants KNDD: 01GI0710, 01GI0711, 01GI0712, 01GI0713, 01GI0714, 01GI0715, 01GI0716; Grants Health Service Research Initiative: 01GY1322A, 01GY1322B, 01GY1322C, 01GY1322D, 01GY1322E, 01GY1322F, 01GY1322G). The publication was also supported by the study “Healthy Aging: Gender specific trajectories into latest life” (AgeDifferent.De) that was funded by the German Federal Ministry of Education and Research (Grants 01GL1714A; 01GL1714B; 01GL1714C; 01GL1714D).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of all research centers involved (approval numbers: Hamburg: OB/08/02, 2817/2007, MC-390/13; Bonn: 050/02; 174/02, 258/07, 369/13;Mannheim: 0226.4/2002, 2007-253E-MA, 2013-662 N-MA; Leipzig: 143/2002, 309/2007, 333-1318112013; Düsseldorf: 2079/2002,2999/2008, 2999; München: 713/02, 713/02 E) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Ethical approval
The ethics committees of all six study centers have approved the study. The study was conducted according to the principles expressed in the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study. The procedures followed were in accordance with the ethical standards of the responsible committees.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buczak-Stec, E., Hajek, A., van den Bussche, H. et al. Frequent attendance in primary care in the oldest old: evidence from the AgeCoDe-AgeQualiDe study. Aging Clin Exp Res 32, 2629–2638 (2020). https://doi.org/10.1007/s40520-020-01495-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01495-2